| disease | Chronic Suppurative Parotitis |
| alias | Chronic Recurrent Parotitis |
Chronic suppurative parotitis (chronic recurrent parotitis) is clinically common. The outcomes differ significantly between adults and children.
bubble_chart Etiology
The cause of chronic recurrent parotitis is not very clear, but it is generally believed that reduced salivary secretion and stasis are important factors. After severe episodes of acute parotitis, the ductal epithelium undergoes mucous metaplasia, increasing the mucus content in saliva, which is one of the factors contributing to salivary stasis. Intra-glandular stones, scar-induced narrowing of the duct orifice due to traumatic inflammation, or an excessively narrow main duct can all lead to dilation distal to the obstruction site, resulting in salivary stasis. Some refer to this as obstructive parotitis. The reason recurrent parotitis frequently occurs in the parotid gland is thought to be due to its longer and narrower ducts, which are more prone to salivary stasis.
Bacterial cultures of mucopurulent saliva from patients with recurrent parotitis often reveal Streptococcus viridans or other weakly pathogenic cocci. Opinions differ on whether these bacteria are the direct cause of parotid infection, with many scholars considering them merely a secondary manifestation.
bubble_chart Clinical Manifestations
Patients often cannot pinpoint the exact onset time and usually seek medical attention due to recurrent episodes of parotid gland swelling. The swelling is frequently bilateral. Swelling episodes may sometimes be related to eating and accompanied by mild pain, which occurs because increased and viscous saliva secretion during meals leads to obstruction. In many cases, the parotid swelling is not clearly related to eating. Patients may wake up feeling a sense of fullness in the parotid gland area, and after slight {|###|}massage, a "salty" fluid may overflow from the duct, providing local relief.
Clinical examination may reveal mild or no noticeable swelling of the parotid gland. In cases of acute infection, the skin may appear slightly red, but it is generally normal. The duct orifice may show mild redness, and pressing the gland may release turbid, "snowflake-like" saliva, thick egg-white-like saliva, or even mucus plugs instead of saliva. In long-standing cases, palpation may reveal a firm gland and a thickened, cord-like parotid duct.Chronic recurrent parotitis typically does not present with systemic symptoms.
Recurrent parotitis in children differs from that in adults. The condition can occur in infants and children up to 15 years of age, with 5-year-old boys being the most commonly affected. Episodes may recur at intervals ranging from weeks to months, with shorter intervals in younger children. As children grow older, the intervals between episodes lengthen, sometimes to once every 1–2 years. The condition tends to resolve spontaneously after adolescence, with very few cases persisting. Swelling can occur suddenly and may be unilateral or bilateral. Sialography often reveals punctate dilatation (sialectasis) of the terminal ducts in both glands, though swelling may occur on only one side. Due to the self-limiting nature of recurrent parotitis in children, many believe it is caused by congenital dysplasia. Several studies have shown that children diagnosed with recurrent parotitis exhibit resolution of the previously observed terminal punctate dilatation upon sialography in adulthood. However, the exact cause remains unclear.
The diagnosis of chronic recurrent parotitis is primarily based on clinical manifestations and sialography. Taking a plain X-ray before the contrast study is necessary to rule out the presence of calculi. The sialographic findings show partial narrowing and partial dilation of the ductal system, resembling sausage-like changes, with spotty dilation of the terminal ducts in the glandular portion. Therefore, this condition is referred to in the literature as chronic punctate parotitis.
The sialographic manifestations of chronic recurrent parotitis and Sjögren's syndrome, now recognized as an autoimmune disease, remain incompletely understood in terms of their relationship and distinctions. Histopathologically, the two differ: chronic recurrent parotitis exhibits acinar atrophy or even disappearance, replaced by proliferative fibrous tissue. The ducts show hyperplasia and dilation with mucous cell metaplasia, accompanied by chronic inflammatory cell infiltration in the surrounding and interstitial tissues. In contrast, Sjögren's syndrome primarily manifests as benign lymphoepithelial lesions.Recurrent parotitis in children must be differentiated from mumps. Mumps has a history of contact, often occurs bilaterally simultaneously, and is accompanied by fever. The parotid duct secretion is normal.
bubble_chart Treatment Measures
The treatment of chronic recurrent parotitis differs between children and adults. For children, it is important to drink plenty of water, perform daily gland massage to aid secretion drainage, and maintain oral hygiene. If acute inflammation is present, antibiotics may be used. The basic principles of treatment for adults with chronic recurrent parotitis are similar, but the therapeutic outcomes are less satisfactory. If causative factors such as stones or duct orifice stenosis are identified, the stones can be removed or the duct orifice can be dilated (using blunt probes inserted carefully into the duct, starting with finer ones and gradually progressing to thicker ones). Medications such as iodized oil or various antibiotics can also be instilled into the duct. If these treatments prove ineffective, surgery may be considered.
There are two surgical approaches: one is duct ligation, which can be performed intraorally (Figure 1). The indication for this procedure requires that the parotid duct system has been repeatedly flushed with antibiotics, and mucopurulent secretions have significantly decreased or ceased. Post-ligation, oral atropine sulfate tablets can be administered, 0.3mg once to three times daily for 3–5 days. Pressure dressing should be applied to the parotid region to promote gland atrophy. The main postoperative complication is spontaneous ulceration of mucopurulent secretions or the formation of retention abscesses. The second surgical method involves conservative treatment and duct ligation failure, in which case a parotid lobectomy with facial nerve preservation may be performed if the patient desires surgery. Due to long-term inflammation, fibrous tissue formation and adhesion to surrounding tissues make facial nerve dissection more challenging. Postoperative deviation of the mouth can be managed with vitamin Bi and B12, combined with physical therapy. It is crucial to remove as much glandular tissue as possible and completely excise the entire parotid duct to prevent retention abscess formation in any remaining duct segments.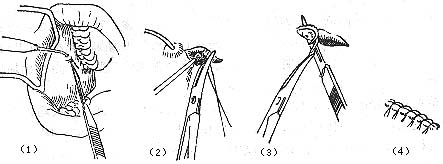
Figure 1: Parotid Duct Ligation
(1) Insert a blunt probe into the parotid duct and incise the buccal mucosa along the duct (2) Free the duct and ligate it (3) Transect the duct and the parotid duct papilla (4) Suture the buccal mucosa




