| disease | Submental and Sublingual Space Infection |
Infection of the multiple spaces of the floor of the mouth, also known as cellulitis of the floor of the mouth, was once considered one of the most severe and difficult-to-treat inflammations in the maxillofacial region. With advancements in diagnosis and treatment, as well as the rational use of effective antibiotics, this condition has become extremely rare in recent years.
bubble_chart Etiology
Below the mandible and between the tongue and hyoid bone, there are multiple muscles whose pathways intersect. Between the muscles and between the muscles and the mandible, loose connective tissue and lymph nodes are abundant. Therefore, the spaces in the floor of the mouth are interconnected (Figure 2). Once cellulitis occurs due to odontogenic or other reasons, it can easily spread to these spaces, leading to extensive cellulitis. Infections involving multiple spaces in the floor of the mouth generally refer to the simultaneous involvement of the bilateral submandibular, sublingual, and submental spaces. The infection may be primarily caused by *Staphylococcus aureus*, resulting in suppurative cellulitis of the floor of the mouth, or it may be caused mainly by anaerobic or necrotizing bacteria, leading to necrotizing cellulitis of the floor of the mouth. The latter is also known as Ludwig's angina, which manifests with severe systemic and local reactions clinically.
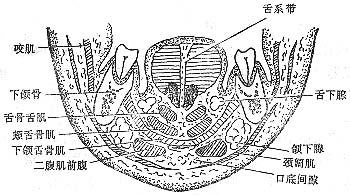
Figure 2 Anatomical location of the spaces in the floor of the mouth
Infections involving multiple spaces in the floor of the mouth can originate from periapical periodontitis of mandibular teeth, periodontal abscesses, subperiosteal abscesses, pericoronitis, osteomyelitis of the jaw, as well as submandibular gland inflammation, lymphadenitis, acute tonsillitis, injuries to the soft tissues of the floor of the mouth, and jaw injuries.
The main pathogens causing suppurative cellulitis of the floor of the mouth are *Staphylococcus* and *Streptococcus*, while the pathogens causing necrotizing cellulitis are primarily anaerobic and necrotizing bacteria. Infections involving multiple spaces in the floor of the mouth often involve mixed bacterial flora, including not only *Staphylococcus* and *Streptococcus* but also *Clostridium perfringens*, anaerobic streptococci, *Clostridium septicum*, *Clostridium oedematiens*, *Clostridium gasogenes*, and *Clostridium histolyticum*, among others.bubble_chart Clinical Manifestations
Suppurative sexually transmitted disease-caused cellulitis of the floor of the mouth. In the initial stage [first stage], swelling mostly occurs in one side of the submandibular or sublingual space. Therefore, the local characteristics resemble those of submandibular or sublingual cellulitis. If the inflammation continues to spread to the entire floor of the mouth around the jaw, diffuse swelling will appear bilaterally in the submandibular, sublingual, and chin areas (Figure 3).
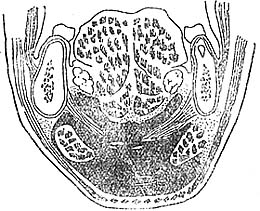
Figure 3 Cellulitis of the floor of the mouth space
Putrid necrotic sexually transmitted disease-caused cellulitis of the floor of the mouth, with very extensive soft tissue edema. The edema can extend upward to the cheeks and downward to the clavicle level of the neck; in severe cases, it may even reach the upper chest. There is spontaneous severe pain around the jaw, a burning sensation, and the skin surface is slightly rough, red, swollen, and hard. The skin in the swollen area appears purplish-red, tender, with obvious pitting edema and no elasticity. As the lesion progresses, deep muscles and other tissues undergo necrosis and liquefaction, leading to fluid accumulation and a sense of mobility. Due to gas production in the subcutaneous tissue, crepitus may be palpable. Upon incision, there is a large amount of coffee bean-colored, thin, foul-smelling, bubble-mixed liquefaction, and the muscle tissue appears dark brown, while the connective tissue is grayish-white, with no obvious bleeding. During the progression of the disease, edema appears in the mucous membrane of the floor of the mouth, and the tongue is pushed upward. Due to tongue stiffness and limited movement, patients often experience slurred speech, difficulty swallowing, and inability to eat normally. If the swelling extends to the base of the tongue, breathing difficulties may occur, making it impossible for the patient to lie flat; in severe cases, dysphoria and restlessness, shortness of breath, cyanosis of the lips, or even the "three depressions" sign may appear, posing a risk of suffocation. In some cases, the infection may spread to the mediastinum, manifesting symptoms of mediastinitis or mediastinal abscess.
Systemic symptoms are often severe, frequently accompanied by fever and shivering, with body temperature reaching above 39–40°C. However, in cases of putrid necrotic cellulitis, due to severe systemic intoxication, body temperature may not rise. Patients exhibit shallow breathing, weak and rapid pulse, and even a drop in blood pressure, leading to shock.bubble_chart Treatment Measures
Ludwig's angina, whether caused by infection from suppurative sexually transmitted disease pathogens or putrefactive necrotic sexually transmitted disease pathogens, presents with severe local and systemic symptoms. The primary dangers are respiratory obstruction and systemic toxicity. In treatment, in addition to the intravenous administration of broad-spectrum antibiotics to control the progression of inflammation, emphasis should also be placed on systemic supportive therapy, such as fluid infusion, blood transfusion, and, when necessary, oxygen administration and maintenance of water-electrolyte balance. Additionally, timely seasonal epidemic incision for decompression and drainage should be performed.
For incision and drainage, the procedure is generally performed externally based on the extent of swelling or the location of abscess formation. Incising at areas where the skin is red and fluctuant is relatively easier. If the local swelling is diffuse or accompanied by secondary edema, and the abscess is deep within the tissue, making it difficult to pinpoint the abscess location, aspiration can be performed first to confirm the abscess site before proceeding with the incision. If the swelling has spread throughout the perimandibular region or if respiratory distress is present, extensive incision should be performed. The incision can be made bilaterally under the mandible and chin, parallel to the mandible, in a "collar" or inverted "T" shape (Figure 1). During the procedure, in addition to widely incising the floor of the mouth, the muscles of the floor of the mouth should be sufficiently separated to ensure adequate drainage of pus from all compartments. If Ludwig's angina is caused by putrefactive necrotic sexually transmitted disease pathogens and the swelling extends to the neck and anterior chest region, with subcutaneous crepitus upon palpation, multiple incisions should be made along the skin lines to widely open the wound, alter the anaerobic environment, and achieve thorough drainage. The wound should then be repeatedly irrigated with 3% hydrogen peroxide or 1:5000 potassium permanganate solution, 4–6 times daily, with a rubber tube left in place for drainage.

Figure 1 Inverted "T" incision for extensive incision of Ludwig's angina.




