| disease | Congenital Vertical Talus |
| alias | Congenital Convex Pes Valgus |
Congenital vertical talus, also known as congenital convex pes valgus, is primarily characterized by a primary dislocation of the talocalcaneonavicular joint. The navicular bone shifts to the dorsal side of the talar neck, locking the talus in a more vertical position, resulting in a rocker-bottom foot deformity.
bubble_chart Pathogenesis
It is generally believed that this deformity is formed within the first three months of embryonic development. Clinically, there are two types: isolated and associated. The latter is often one of the deformities in congenital diseases such as spina bifida, multiple joint contractures, neurofibromatosis, trisomy 13-15, 18, etc. The cause of isolated vertical talus is still unclear. Some suggest that it is due to arrested development of the foot embryo. Bitsila conducted experiments on young rabbits by simultaneously severing the extensor digitorum longus, tibialis anterior, and transverse ligament of the leg, and shortening the gastrocnemius, successfully creating an animal model of vertical talus. Therefore, he proposed that primary soft tissue lesions are the main factors causing this deformity. Other scholars have found that the incidence in certain families and twins is significantly higher than in the general population, suggesting a genetic factor.
Pathological changes can be divided into bony deformities and soft tissue lesions. The bony deformity mainly involves the navicular bone and the dorsal side of the talar neck forming a joint, locking the talus in a vertical position. The upper part of the talar head is flattened or oval, the talar neck is hypoplastic and shortened, and a joint surface is formed on the dorsal side. The proximal articular surface of the navicular bone tilts toward the metatarsal side. The calcaneus is displaced posterolaterally. The anterior part of the calcaneus deviates laterally and flexes toward the metatarsal side. The sustentaculum tali is hypoplastic and loses its support function for the talus. The lateral column of the foot is depressed, and the medial column is relatively elongated.
There are also significant changes in the soft tissues. Contracture of the tibionavicular ligament and the dorsal talonavicular ligament are the main factors affecting reduction. Contracture of the bifurcate ligament causes abduction of the foot. Contracture of the interosseous talocalcaneal ligament and the calcaneofibular ligament hinders the reduction of the calcaneus's posterolateral displacement. The calcaneonavicular metatarsal ligament, the talonavicular metatarsal ligament, and the medial joint capsule are elongated. The tibialis anterior, extensor digitorum longus, extensor hallucis longus, peroneus brevis, and triceps surae muscles have increased tension due to contracture. The peroneus longus and tibialis posterior tendons move anteriorly to the ankle, acting as dorsiflexors (Figure 1).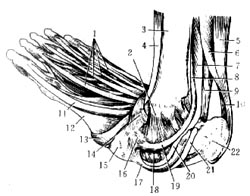
Figure 1 Congenital vertical talus and abnormal changes in tendons (1. Extensor digitorum tendon 2. Deltoid ligament 3. Tibia 4. Tibialis anterior 5. Gastrocnemius 6. Soleus 7. Flexor digitorum longus 8. Tibialis posterior 9. Flexor hallucis longus 10. Achilles tendon 11. Extensor hallucis longus 12. First metatarsal bone 13. Tibialis anterior tendon 14. Cruciate ligament 15. First cuneiform bone 16. Navicular bone 17. Calcaneonavicular metatarsal ligament 18. Talar head 19. Tibialis posterior tendon 20. Flexor digitorum longus tendon 21. Flexor hallucis longus tendon 22. Calcaneus)
bubble_chart Clinical Manifestations
The characteristic clubfoot deformity can be detected immediately after the child's birth. The sole of the foot is convex, presenting a "rocker-bottom" appearance. The forefoot is abducted and dorsiflexed, with the talar head protruding medially on the plantar side, while the hindfoot is fixed in a position of metatarsus flexion and eversion. Increased tension in the tibialis anterior, extensor digitorum longus, and peroneus longus and brevis muscles restricts the forefoot's ability to flex and invert. Contracture of the triceps surae exacerbates calcaneal eversion and metatarsus flexion deformity, and hinders dorsiflexion of the ankle joint.
The age at which the child begins to walk is usually not delayed, but the gait is clumsy. When standing, the forefoot is noticeably abducted, with the talar head and calcaneus bearing weight in an everted position, but the posterior part of the calcaneus often does not touch the ground.X-ray examination on the lateral view shows the talus in a vertical position, almost parallel to the longitudinal axis of the tibia. The talus is in a position of metatarsus flexion, with significant dorsiflexion of the forefoot at the midtarsal joint. Since the ossification center of the navicular bone does not appear before the age of 3, the axis of the first cuneiform is used to estimate the position of the navicular bone. If this line extends posteriorly to the dorsal side of the talar head, it indicates dorsal dislocation of the navicular bone. On a lateral view with forced dorsiflexion, the talar axis in a normal child's foot passes through the lower half of the cuboid, while the calcaneal axis passes through the upper half of the cuboid. In congenital vertical talus, the talar axis shifts toward the to be decocted later side of the cuboid, sometimes passing anterior to the calcaneus, and the calcaneal axis also shifts toward the metatarsus side of the cuboid (Figure 2). On the anteroposterior view, the talocalcaneal angle is significantly increased (normal range: 20°–40°). After the ossification of the navicular bone appears, its displacement to the dorsal side of the talar neck can be observed.

Figure 2 A. Lateral view of a normal foot showing the talocalcaneal angle and tibiotalar angle
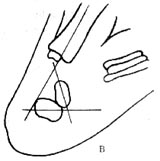
Figure 2 B. Congenital vertical talus with significantly reduced talocalcaneal and tibiotalar angles, and the calcaneal axis shifted toward the metatarsus side of the cuboid.
bubble_chart Treatment MeasuresDue to the rigidity of this deformity, the earlier the treatment, the better. It is generally believed that the best time to treat this condition is within three weeks after birth, and manual reduction may be successful. The sequence of manual reduction is as follows: first, passively stretch the gastrocnemius and calcaneofibular ligament. The operator pulls the heel distally and medially with one hand, while pushing the front of the calcaneus with the other hand, maintaining this for 10 seconds. Then, pull the forefoot toward the metatarsus side, invert and adduct it to stretch the dorsiflexion and eversion muscles. Next, pull the forefoot distally to stretch the tibionavicular and talonavicular ligaments, gradually adducting and inverting the forefoot. Each maneuver should be held for 10 seconds, and each session should last 15 minutes. Finally, fix with a long-leg gypsum cast, maintaining the forefoot in metatarsal flexion and inversion, and the hindfoot in dorsiflexion. The gypsum cast is typically changed every 2-3 days, and the manual reduction steps are repeated to stretch the contracted soft tissues. After approximately 4-6 weeks, closed reduction can be attempted. Begin by pulling the forefoot and navicular bone in the direction of the deformity, positioning the navicular bone above the talar head and the calcaneus below the talus. Then, push the talar head dorsally from the medial side of the foot, pull the heel to invert it, and simultaneously flex and invert the forefoot metatarsus to restore the normal anatomical relationship of the talonavicular joint. After confirming successful reduction via X-ray, insert a Kirschner wire through the first and second toes to fix the cuneiform, navicular, and talus bones, and apply a long-leg gypsum cast. Initially, maintain the forefoot in metatarsal flexion and inversion, and the hindfoot and ankle in metatarsal flexion. Change the gypsum cast every 2-3 weeks, gradually dorsiflexing the affected foot. Typically, the gypsum cast is used for 8-10 weeks.
If closed reduction is unsatisfactory and the child is three months old, open reduction should be performed. The surgery involves releasing the contracted joint capsule and ligaments, including: ① the dorsal and lateral parts of the talonavicular ligament; ② the tibionavicular ligament and bifurcate ligament; ③ the dorsal and lateral parts of the calcaneocuboid joint capsule; ④ the calcaneofibular ligament and interosseous talocalcaneal ligament. At the same time, lengthen the contracted tendons, such as the Achilles tendon, tibialis anterior tendon, extensor digitorum longus tendon, and peroneus longus and brevis tendons. Then, under direct vision, reduce the talonavicular joint and restore the normal alignment of the foot. Fix the cuneiform, navicular, and talus bones with a Kirschner wire. Tighten and suture the calcaneonavicular metatarsal ligament, the metatarsal and medial parts of the talonavicular joint capsule, and shift the tibialis posterior tendon distally to fix it on the metatarsal side of the first cuneiform. Postoperatively, apply a long-leg gypsum cast for 8-12 weeks. The Kirschner wire is usually removed six weeks after surgery.
If treatment begins after the child is four years old, the medial column of the foot will have significantly elongated, hindering the reduction of the talonavicular joint. During open reduction, the dorsally displaced navicular bone should be excised to allow the first cuneiform to articulate with the talar head. Over time, through growth and remodeling, the talar head will occupy the space left by the excised navicular bone. If the child is older than eight years and has not been treated, open reduction and navicular excision are not only difficult to succeed but also prone to complications such as talar necrosis. Therefore, it is advisable to delay treatment until after the age of 10, when a three-pass arthrodesis can be performed.
Congenital vertical talus has characteristic manifestations, with a convex sole resembling a boat shape and forefoot abduction, which can be detected at birth, making it easily distinguishable from common congenital equinovarus. Certain neuromuscular diseases, such as poliomyelitis and multiple arthrogryposis, can also produce convex valgus foot deformities. However, acquired convex valgus foot appears later and has other manifestations of the primary disease, making it not difficult to differentiate from this condition.




