| disease | Congenital Choanal Atresia |
This disease is a severe nasal deformity and belongs to a familial hereditary disorder. According to Evans (1971), among 65 cases of congenital choanal atresia, 28 cases (43%) were associated with other congenital malformations, including multiple congenital anomalies (CHARGE syndrome), such as coloboma of the iris, congenital heart anomalies, congenital choanal atresia, retarded growth, genital hypoplasia, and ear anomalies. Additionally, other malformations may be present, such as strabismus, iris paralysis, maxillofacial osteogenesis imperfecta syndrome, atresia of the external auditory canal, ileal diverticulum, intestinal malposition, urinary system malformations, and polydactyly of the foot.
bubble_chart Etiology
Most scholars believe that congenital choanal atresia occurs during the 6th day-night cycle of embryonic development, when the mesenchymal tissue in the bucconasal cavity is too thick to be absorbed and fails to penetrate and connect with the oral cavity, forming the primitive choana and resulting in an atretic septum. This septum may be membranous, bony, or mixed. The atretic septum can be as thin as paper or as thick as 12mm, but is typically around 2mm. Small perforations may also form within it, but with insufficient ventilation, this is termed incomplete atresia. The position of the atretic septum is classified into anterior margin atresia and posterior margin atresia, often located at the junction of the soft and hard palate near the choanal edge, tilting upward and backward, attached to the sphenoid body, externally connected to the medial pterygoid plate of the sphenoid bone, internally to the vomer, and inferiorly to the palatine bone. Both surfaces of the atretic septum are covered with nasal mucosa.
bubble_chart Clinical ManifestationsChildren with bilateral choanal atresia experience periodic breathing difficulties and cyanosis immediately after birth, gradually adapting to mouth breathing after about 4 weeks. However, they still face breathing difficulties during feeding and require additional time to learn the coordination of alternating between breathing and sucking. Consequently, there is a risk of asphyxia after birth and severe consequences of malnutrition.
During childhood and adulthood, the main symptoms include nasal obstruction, snoring, and sleep apnea syndrome during sleep, frequent drowsiness, closed nasal speech due to mouth breathing, as well as dry throat and poor thoracic development. Unilateral choanal atresia does not threaten life; as the child grows, only one nasal passage remains obstructed, leading to secretion retention on the affected side.
When a newborn presents with peripheral respiratory distress, cyanosis, and feeding difficulties, this condition should be considered. The following methods can be used for diagnosis:
1. Attempt to pass a thin rubber catheter from the anterior nostril into the nasopharynx. If the catheter encounters an obstruction before reaching 32 mm into the oropharynx and the catheter is not visible on examination of the posterior oropharyngeal wall, a diagnosis of choanal atresia can be made. Care must be taken to rule out the possibility that the catheter is too soft or incorrectly directed, causing it to coil in the nasal cavity and fail to reach the posterior nostril.
2. Insert a cotton-tipped applicator along the nasal floor from the anterior nostril to detect the location and nature of the obstruction.
3. Instill methylene blue or 1% Chinese Gentian violet solution into the nasal cavity and observe whether the oropharynx becomes stained after 1–2 minutes. If no staining is observed, the condition can be diagnosed.4. Slowly instill iodized oil into the nasal cavity for X-ray contrast imaging, which can reveal the presence and depth of choanal atresia.
5. Nasal endoscopy: Use a 0-degree fiber-optic nasal endoscope inserted into the anterior nostril while suctioning secretions to observe the posterior nostril. This method not only diagnoses the condition but also helps exclude other causes of nasal obstruction, such as congenital intranasal meningoencephalocele, nasal polyps, adenoid hypertrophy, nasopharyngeal tumors, foreign bodies, cicatricial stenosis, and deviated nasal septum.
bubble_chart Treatment Measures
(1) General Emergency Measures After the birth of a newborn, if bilateral congenital choanal atresia is diagnosed, it should be treated as an emergency to maintain airway patency, prevent suffocation, and ensure nutrition. A rubber nipple can be used by cutting off its tip and inserting it into the mouth, securing it to the head with a strap to facilitate oral breathing. A small amount of milk can be dripped through the nipple. The nipple can be removed once the infant becomes accustomed to oral breathing. It is best to have dedicated care to prevent suffocation, and attention should be paid to nutritional intake.
(2) Surgical Treatment Surgical removal of the atretic septum can be performed via four approaches: transnasal, transpalatal, transseptal, or transmaxillary sinus. The choice depends on the child's age, severity of symptoms, nature and thickness of the septum, and overall condition. For safety, a tracheostomy is recommended first.
1. Transnasal Approach Suitable for cases where the nasal cavity is wide enough to visualize the atretic septum, membranous or thin bony septa, newborns, or children in poor general condition requiring urgent restoration of nasal breathing.(1) Anesthesia General anesthesia for children and local surface anesthesia for adults.
(2) Incision A "["-shaped incision is made on the left nasal septum and a "]"-shaped incision on the right nasal septum. The mucous membrane is dissected to expose the bony surface.
(3) Septum Removal The bony septum is removed using a chisel, curette, or electric drill, preserving the mucous membrane on the posterior (pharyngeal) side to cover the lateral bone surface. The posterior end of the nasal septum must be excised to connect the openings on both sides. The size of the opening should allow passage of an index finger. A corresponding-sized rubber or plastic tube is then inserted, or a balloon may be used for fixation. The duration of placement depends on the nature of the septum: two weeks for membranous septa and 4–6 weeks for bony septa. To prevent restenosis, periodic dilation may be performed within a year. This procedure is more convenient when performed under fiber-optic nasal endoscopy.
For newborns, a small mastoid curette can be used to scrape along the nasal floor, rotating to remove the bony septum to an adequate size while preserving the posterior mucous membrane. A cross-shaped incision can be made, and a rubber tube can be pulled retrograde from the nasopharynx to fix the mucosal flap onto the bone surface.
During the transnasal approach, care must be taken to avoid injury to the descending palatine artery, skull base, and cervical spine.
2. Transpalatal Approach The advantage is excellent surgical exposure, direct visualization of the lesion, complete removal of the septum, and optimal use of mucous membrane to cover the wound. Suitable for thicker atretic septa.
(1) Position and Anesthesia The child is placed supine with the head extended backward. A 0.1% adrenaline cotton pad is placed against the anterior wall of the atretic septum in the deep nasal cavity. A small amount of 1% procaine with adrenaline is injected at the junction of the hard and soft palate to reduce intraoperative bleeding. General anesthesia is administered via tracheostomy.
(2) Incision An Owens semicircular incision is made on the hard palate, cutting through the mucous membrane, with the ends extending posteriorly to the maxillary tuberosity. The mucoperiosteal flap is dissected to the edge of the hard palate (Figure 1).
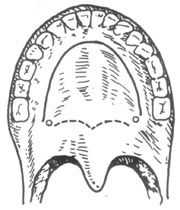
Figure 1: Semicircular incision (Owens incision)
(3) After exposing the posterior edge of the hard palate, a thick suture is passed through the freed mucoperiosteal flap for posterior traction (Figure 2).
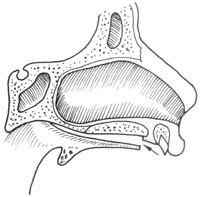
Figure 2: Dissection of the mucoperiosteal flap to the posterior edge of the hard palate, followed by freeing the posterior mucous membrane along the back of the bony septum.
(4) Remove the atresia interval. Separate the nasal floor mucosa on the posterior side of the hard palate (nasal floor surface). Use rongeurs to remove part of the posterior edge of the palatal bone on the affected side, revealing the bony septum slanting toward the sphenoid body. Separate the mucosa behind the bony septum, chisel away the septum, and then remove a portion of the vomer along its posterior edge using the method of submucosal resection of the nasal septum to maximally enlarge the posterior nasal aperture and ensure patency. The mucosa anterior and posterior to the bony septum and at the posterior end of the nasal septum can be used to cover the exposed bone surfaces (Figure 3).
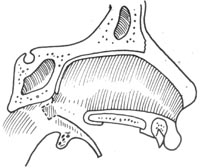
Figure 3 Remove the bony septum, incise the anterior membranous adhesion, and use the membranous adhesion to cover the lateral wall
(5) Suture the incision Reposition the mucoperiosteal flap of the hard palate incision and suture it tightly with fine silk thread. If there is any tearing near the soft palate, it should also be sutured meticulously to avoid postoperative perforation. Finally, insert a rubber or plastic tube through the anterior nostril to secure the trimmed nasal mucosal membrane. Remove the rubber tube after 4 weeks and schedule regular follow-ups. If postoperative adhesions occur in the posterior nasal aperture, they should be addressed promptly, with dilation performed if necessary (Figure 4).
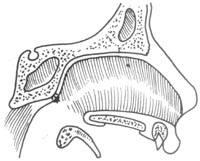
Figure 4 Thin the posterior membranous adhesion of the bony septum, attach it to cover the roof, and finally reposition and suture the hard palate mucoperiosteal flap
3. Transnasal Septal Approach This method is only suitable for treating choanal atresia in adults. It can be used for unilateral, bilateral, membranous, or bony cases.
(1) Position and anesthesia Same as submucous resection of the nasal septum.
(2) Incision Use a Killian incision or make a slightly posterior incision.
(3) Elevate the mucoperiosteum The extent should be as wide as possible, especially superiorly and inferiorly, and may include the mucosal membrane of both nasal floors to expand the posterior field of view.
(4) Incise the nasal septal cartilage and elevate the mucoperiosteum on the opposite side of the nasal septum, extending the dissection as widely as possible. When dissecting posteriorly, part of the nasal septal cartilage and perpendicular plate of the ethmoid bone can be removed. Upon encountering the bony septum, use a chisel to remove it until the anterior wall of the sphenoid sinus is visible. Finally, insert a rubber or plastic tube through the anterior nostril to prevent choanal adhesions. Postoperative periodic dilation may be performed if necessary.
4. Transmaxillary Sinus Approach This method is only suitable for unilateral choanal atresia in adults. It utilizes the de Lima procedure to open the posterior ethmoid sinus via the maxillary sinus, reaching the choanal region to excise the atretic septum.




