| disease | Third-degree Perineal Tear |
| alias | Complete Perineal Laceration |
A third-degree perineal tear, also known as a complete perineal tear, includes lacerations of the vaginal opening, perineum, and anal sphincter. In severe cases, the tear may extend to the rectal wall, leading to fecal and gas incontinence. The primary cause is often improper management during childbirth, though it can occasionally result from trauma. With the widespread implementation of modern delivery techniques and proper perineal protection by midwives, the incidence of third-degree perineal tears has significantly decreased. However, such cases still occur occasionally in large urban hospitals.
bubble_chart Etiology
During labor observation, it is crucial to accurately estimate fetal size, understand fetal position and presentation, and prevent precipitous delivery. For mothers with occiput posterior position and outlet stenosis requiring forceps-assisted delivery, a large episiotomy must be performed, and bilateral episiotomy may be necessary when needed, while ensuring perineal protection. Median episiotomy has its advantages when performed by skilled practitioners; however, when performed by less experienced operators with inadequate perineal protection, the median episiotomy incision may extend posteriorly, leading to third-degree perineal tears, which warrants special attention.
bubble_chart Clinical Manifestations
A third-degree perineal tear occurs during the second stage of labor, when the fetal head is crowning, and the midwife may sense a tearing sensation in the perineum. The third-degree tear is identified and sutured immediately after childbirth. Due to varying degrees of rupture, symptoms can range from mild to severe. For instance, if only part of the sphincter is torn, the patient may lose control only when stools are loose or when passing gas. In such cases, the patient tries to maintain dry stools. Bowel control primarily relies on the anal sphincter, which prevents sudden leakage when intra-abdominal pressure increases. However, voluntary control of bowel movements depends not only on the sphincter but also on the levator ani muscle. In severe cases, even dry stools cannot be controlled, and the vulva is frequently soiled by feces. We had a 43-year-old patient who could control dry stools but complained of bright red blood in her stool for two years, which was caused by rectal mucosal injury.
Upon examination, the perineum was found to be absent, with the vagina and the distal end of the rectum connected. The skin behind the anus showed radial wrinkles, and the retracted ends of the sphincter formed small depressions on either side of the anus. During a rectal exam, the patient was instructed to contract inward to test the sphincter's control function. If the rectum is also torn, the rectal mucosa appears red and protrudes outward.(1) Perineal tears during childbirth: Third-degree perineal tears occur during the second stage of labor, when the fetal head is crowning. The midwife may sense a tearing sensation in the perineal area. If a third-degree tear is identified and sutured immediately after childbirth, the wound generally heals well.
(2) Old perineal tears: During examination, insert a finger into the anus and instruct the patient to contract inward as if holding back a bowel movement. At this time, the examining finger will not sense the contraction of the sphincter muscle. Due to retraction of the torn muscle ends, a small depression can be observed on the side of the anus, and the circular ends of the torn muscle can be located at the tear site.
bubble_chart Treatment Measures
Surgical Repair
(1) Repair of Tears During Childbirth The repair of perineal tears during childbirth, also known as the repair method for fresh third-degree perineal tears. Timing of repair: It should be performed immediately after the delivery of the placenta, provided the patient's general condition permits; otherwise, the repair can be postponed for 12–24 hours.
1. Key Points During Surgery Fresh wounds lack scar tissue and heal easily, but sometimes the torn muscles are disorganized, so the layers must be clearly identified. Avoid excessive freeing of the rectal wall. If the sphincter muscle is strong, silk sutures or No. 2 chromic catgut can be used. Since there is no preoperative bowel preparation, the wound is prone to infection. When repairing the anterior rectal wall, the first layer of sutures must not penetrate the rectal mucosa. If the suture passes through the mucosa and knots are tied inside the rectal lumen, the most critical step is the first suture. If visibility is poor, a finger can be placed inside the rectum as a guide. For suturing the sphincter, No. 2 chromic catgut or medium silk sutures can be used. First, lift the sphincter to test its strength. After completing the suturing of the levator ani muscle, proceed to suture the sphincter from the inside outward for easier operation. Before suturing the vaginal wall, rinse the wound with saline. Antibiotics can be injected around the wound to reduce the risk of infection.
2. Postoperative Management The postoperative care for tears repaired during childbirth is largely the same as for old tears: ① If the patient is transferred from another hospital and the external procedures are unclear, administer 1,500 units of tetanus antitoxin (TAT) intramuscularly first; ② Postoperative bed rest, a residue-free diet, and an indwelling catheter (connected to a sterilized bottle) for 5 days to avoid wound contamination; ③ Oral administration of 1.0 g of streptomycin daily for 5 days to sterilize the bowel; ④ Oral administration of 2 mL of compound tincture of camphor three times daily for 3 days to prevent bowel movements within the first three postoperative days; ⑤ If no bowel movement occurs by the fifth day, administer 30 mL of liquid paraffin orally or perform an oil enema. The enema must be performed by the surgeon personally to avoid rough handling and accidental perforation of the wound by the rectal tube; ⑥ Remove sutures 5–7 days postoperatively.(2) Repair of Old Tears If the wound from a tear repaired during childbirth heals poorly, or if a postpartum perineal tear goes unnoticed, it becomes an old (third-degree) tear. The repair should be delayed until at least 6 months postpartum.
There are two common surgical repair methods: ① The layered method; ② The mucosal flap method. The layered method is often used for fresh third-degree tears.
(1) Layered Method The surgical steps are as follows: Disinfection of the vulva and vagina: Scrub the vulva and vagina with soapy water and gauze, rinse thoroughly with clean water, and then rinse again with 1:1000 benzalkonium bromide solution. Place a gauze roll in the rectum to prevent spillage of intestinal secretions. Before incising the vaginal wall, disinfect again with 75% alcohol.
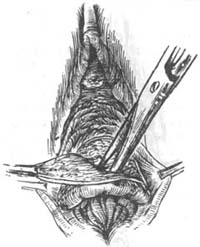
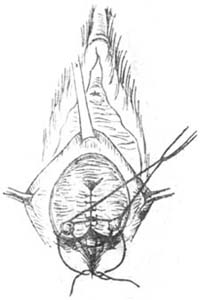
Exposure of the surgical field: Drape with sterile sheets, and suture the labia minora to the labia majora and sterile sheets to keep them separated.Incision: Use tissue forceps to grasp the torn end of the rectovaginal wall. Make an incision at the junction of the vaginal mucosa and rectal mucosa, extending laterally to the depressions on either side of the anus, i.e., the lateral side of the retracted ends of the anal sphincter (Figure 1 (1) ). Trim away any remaining scar tissue.

(1)
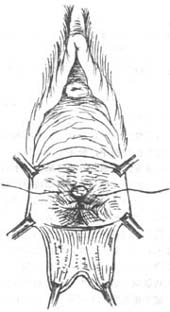
(2)
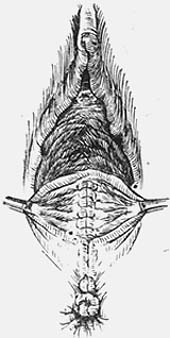
(3)
Figure 1 Repair of Third-Degree Perineal Tear—Layered Method
(1) Incision (2) Locating the Anal Sphincter (3) Suturing the Anal Sphincter
Separate the vaginal wall and rectal wall: Use tissue forceps to retract the vaginal wall. Insert curved blunt scissors into the interface between the vagina and rectum, with the blunt end facing forward. While pushing upward, open the blunt end to separate the vaginal wall and rectal wall along the midline. Cover fingers with gauze and dissect upward and laterally to mobilize the rectum as much as possible. A wider dissected area reduces tension when suturing the rectal wall, preventing suture line dehiscence and promoting healing.
Repair of the anterior rectal wall: The first layer is sutured with interrupted 00 chromic catgut sutures, without penetrating the mucosa. The first stitch is the most important and should be placed above the apex of the wound, the second stitch at the apex, with interrupted sutures spaced approximately 1/2 cm apart. The second layer uses a continuous Lembert suture, starting above the first stitch of the first layer to reinforce and bury the first layer. It is preferable to add a third layer, including some muscle fibers and connective tissue, to invert the second layer and push the rectum posteriorly.
Locating the severed ends of the anal sphincter (Figure 1 (2)). The retracted ends of the anal sphincter can be found in the depression of the anal skin folds. First, use curved hemostatic forceps to separate a space in the subcutaneous tissue; then insert tissue forceps into this space to grasp the severed ends of the sphincter in one attempt, avoiding multiple pulls that could damage the remaining muscle fibers. After locating the ends on both sides, pull them toward the midline. Insert a finger into the anus to assess whether the anal sphincter tightens around it. The sphincter is sutured with 2-3 medium silk sutures (Figure 1 (3)). Sphincter repair can be performed after step (7), as suturing the sphincter first may narrow the external opening, hindering the internal levator ani muscle repair.
Suture the levator ani muscles symmetrically.
Proceed with the posterior vaginal wall repair, paying attention to reconstructing the perineal body.
(2) Mucosal flap method: This technique does not require suturing the rectal wall, reducing the risk of infection. It is advantageous for cases with a wider rectal defect or significant scarring, where layered sutures would create excessive tension and impair healing. However, it is suitable only for shorter rectal wall tears. If the tear is long, the mucosal flap required to cover it may compromise distal blood circulation. The steps are as follows:
① Disinfect the vulva.
② Expose the surgical field.
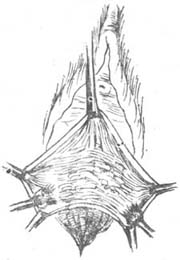
③ Vaginal incision and dissection of the vaginal mucosal flap (Figure 2 (1)(2)): Make an inverted V-shaped incision on the posterior vaginal wall, resembling a "semicircle," with the lower ends of the incision lateral to the depression of the anal skin folds. Insert the left index finger into the vagina, with the thumb outside, and use tissue forceps to retract the vaginal mucosa outward. Cover the fingers with gauze and dissect the vaginal wall downward until beyond the end of the tear, avoiding excessive thinning or perforation of the mucosal flap. This step must be performed carefully; if the mucosa is perforated midway, the procedure must be abandoned and switched to the layered method.
|
|
|
| (1) | (2) |
|
|
|
| (3) | (4) |
|
| |
(5) | |
Figure 2 Perineal third-degree laceration repair—membrane flap method
(1) Vaginal incision (2) Dissection of the membrane flap (3) Suture of the anal sphincter
(4) Approximation of the levator ani muscle (5) Completion of the operation, with the remaining membrane flap protruding anterior to the anus
Locate and suture the anal sphincter, and suture the levator ani muscle, etc. The following steps are the same as the layered method (Figure 2 (3)(4) ).
After the operation is completed, the excess membrane may protrude externally in front of the new anus, resembling hemorrhoids (Figure 2 (5) ). At this time, it is not advisable to trim the membrane short, but the rough surfaces can be approximated. Postoperatively, the membrane may retract. Occasionally, patients may feel discomfort from the protrusion, which can be excised under local anesthesia.
3. Precautions To avoid surgical failure, the following points must be noted: ① Infection leading to wound dehiscence. The surgical field is around the anus, and the surgeon often needs to insert a finger into the rectum for guidance. Therefore, preoperative bowel preparation is essential. Place gauze in the rectum preoperatively, change gloves after the anal finger is withdrawn, and immediately wipe the perianal area from front to back with alcohol gauze. Before suturing the vaginal wall, rinse the wound with sterile saline. For patients with a higher risk of bleeding or infection, a rubber drain can be placed during vaginal wall suturing and removed after 48 hours. ② In the layered method, rectovaginal fistulas often occur at the apex, so the first and second sutures at the apex are crucial. Additionally, ensure sufficient mobilization of the rectal surface to avoid excessive tension on the sutures. ③ Due to prolonged laceration, atrophy of the sphincter or formation of scar tissue may lead to poor sphincter function. Therefore, several days before surgery, the sphincter should be tested by traction at the anal skin fold to assess its function. During surgery, the sphincter should be tested again at this site. If the sphincter cannot be sutured, the levator ani and perineal body muscles must be adequately sutured to ensure effective fecal control. ④ Postoperatively, although fecal control may be restored, the vaginal opening may appear directly connected to the anus without a perineal body. During surgery, attention should be paid to suturing the perineal body muscles in two layers to form a right angle between the vaginal mucosal surface and the perineal skin. ⑤ In cases of repeated repair failures, a subcutaneous incision of the anal sphincter can be performed to reduce wound tension and muscle spasticity. The incision is typically made at the 5 o'clock position. Clinical practice has shown this method to be effective.
4. Preoperative preparation Timing of surgery: Vaginal repair is best performed in women who have completed childbearing. Patients with cough or anemia should first receive treatment for cough and correction of anemia. The surgery should be scheduled after menstruation, as immediate postoperative menstruation may increase the risk of wound infection.
One week before the repair, start administering succinylsulfathiazole four times daily, 2g each time. Succinylsulfathiazole has antiseptic and mild laxative effects on the gastrointestinal tract, preventing infection and facilitating postoperative bowel movements. If succinylsulfathiazole is unavailable, oral streptomycin 1g daily or neomycin 1g daily can be used.
For perimenopausal or postmenopausal women, a small amount of estrogen can be administered one week before surgery to improve vaginal blood circulation, promote epithelial growth, and enhance healing.
Three days before surgery, provide a low-residue semi-liquid diet. Three days before surgery, irrigate the vagina with 0.25% iodine solution twice daily. Sitz baths with 0.4% potassium permanganate should be taken twice daily. Perform a cleansing enema one day before surgery.
5. Postoperative management Continue administering succinylsulfathiazole for one week, or use streptomycin or neomycin. Continue a small dose of estrogen for one week to avoid withdrawal bleeding within the first week. Maintain a low-residue semi-liquid diet for five days.
Keep the wound clean, use perineal alcohol gauze pads, retain the indwelling catheter for 5 days, and clean the wound with alcohol after bowel movements.
No enema is allowed after surgery. If there is still no bowel movement after 5 days postoperatively, a mild laxative can be administered, such as 5mg of bisacodyl or 30ml of oral liquid paraffin. If the stool remains dry, a rubber catheter can be lubricated and inserted along the posterior wall into the rectum to instill 30ml of oil. To prevent fecal impaction in the rectum, a daily rectal examination may be performed (using ample lubricant is essential).
If there is excessive vaginal discharge with an odor, it indicates infection in the vaginal wound. In such cases, the vagina can be irrigated with hot 0.4% potassium permanganate solution. Generally, hot potassium permanganate sitz baths can be started 7 days postoperatively to promote wound healing.
6. Repair after recurrence The causes of recurrence are often insufficient tissue support, estrogen deficiency, inadequate protein nutrition, anemia, or chronic cough, which impair healing. Postoperative perineal exercises are crucial. The primary exercise methods involve tightening the rectum as if holding back a bowel movement or suddenly tightening to interrupt urination during voiding. If reoperation is necessary, it should generally be delayed for 3–6 months to allow inflammation and infection to subside. Alternatively, adrenal corticosteroids and antibiotics may be used to expedite the timing of surgery.
To address the disease-causing factors, effective preventive measures can significantly reduce the incidence rate. The preventive measures are as follows:
① Implement family planning. Multiple pregnancies and deliveries inevitably lead to relaxation and tearing of the pelvic floor muscles; ② Immediately repair perineal tears after childbirth to prevent wound infection and impaired healing; ③ For first-time deliveries with a tight perineum, if the presenting part remains in the perineal area for an extended period, an episiotomy should be performed to avoid submucosal muscle tears or pressure necrosis; ④ During the puerperium period, physical therapy can generally begin the day after childbirth to improve blood circulation in the small pelvis, enhance local muscle tone, strengthen overall health, and avoid heavy physical labor or persistent cough.